Hepatobiliary Disease
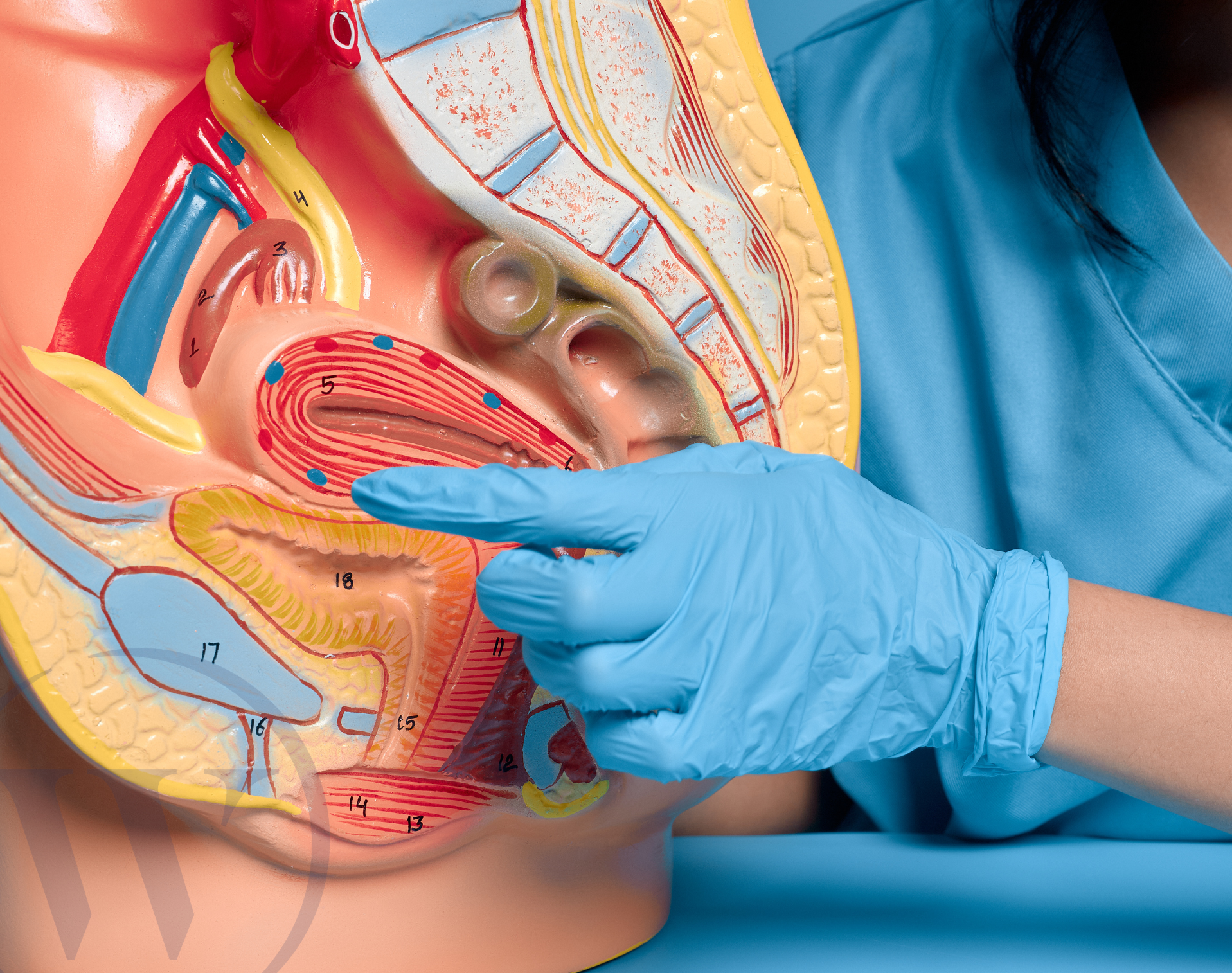
Hepatobiliary disease is a term to describe conditions that affect the organs and structures of the biliary system – the liver, gallbladder and bile ducts.
What is hepatobiliary disease?
Hepatobiliary disease is a catch-all term for any condition or disorder that affects the liver, gallbladder and bile ducts. These diseases can include minor infections, cysts, gallstones, liver cirrhosis, abnormal growths and cancer.
Hepatobiliary disease can be caused by a range of things, including viral, bacterial or parasitic infections, neoplasia (abnormal cell growth), toxic chemicals, alcohol consumption, poor nutrition, metabolic disorders and cardiac failure.
At Welbeck, our consultant gastroenterologists are experts in hepatobiliary disease care, ensuring you receive the world-class treatment you need to make the best possible recovery.
Liver disease
Your liver performs hundreds of functions required to sustain life. It's also a gland because it makes proteins and hormones that other parts of the body need.
Some of the key roles of the liver are:
blood detoxification and purification
bile production (used in digestion)
metabolism of proteins, carbohydrates and fats for energy
regulating blood sugar levels
blood clotting
regulating the amount of blood in the body
storage of vitamins, minerals, fat, and sugar
bile production for digestion of fats and removal of waste from the body.
immune response
hormone production
bilirubin removal
Hepatobiliary disease can affect the health and function of the liver, which can have a widespread impact throughout the entire body.
Most people with liver problems don’t have any symptoms at all. Blockages of the bile ducts can cause abdominal pain. In the severest forms of both conditions, complications can include jaundice (where too much bilirubin has built up in the blood and the skin and whites of the eyes turn yellow), or other symptoms of liver failure, including:
ascites (a build-up of fluid in the belly area),
itchy skin,
loss of appetite and weight loss,
feeling or being sick
abdominal pain
swollen legs or ankles and weakness and fatigue
Common liver diseases
Some of the most common liver diseases are:
alcoholic fatty liver disease (ArLD)
fatty liver disease (metabolic associated steatotic liver disease (MASLD)
inflammation of the liver (hepatitis A, B, C, E, medication-induced liver injury or autoimmune hepatitis)
scarring of the liver (cirrhosis)
haemochromatosis (a genetic condition causing high iron levels)
benign (non-cancerous) and malignant (cancerous) tumours
Diagnosing liver diseases
How liver disease is diagnosed depends on the symptoms you are experiencing. At a consultation, your Welbeck specialist will take a medical history and ask you questions to build a picture of your overall health.
They may then perform one or a combination of the following diagnostic tests:
blood tests to measure liver function, look for signs of abnormal blood clotting and check for high levels of alpha-fetoprotein (AFP), a protein which can indicate liver cancer, other cancers, liver disease, active liver inflammation and hepatitis
imaging scans such as ultrasound, MRI scan, CT scan and FibroScan to evaluate the size and structure of your liver and identify any abnormalities, such as scarring or growths
biopsy to remove a small piece of the tissue from the liver and evaluate the cells under a microscope to make or confirm a diagnosis
Gallbladder disease
Your gallbladder is a small organ that sits just under your liver. Its key function is to store and release the fat-digesting bile produced by the liver.
It’s connected to other parts of your digestive system through a series of bile ducts called the biliary system, which carries bile from your liver to your small intestine, where it helps to break down and digest food.
If your gallbladder is infected or blocked, bile can become backed up in the biliary system affecting the function of the gallbladder, bile ducts, liver and pancreas.
The symptoms of gallbladder problems can vary but can include upper right or upper mid abdominal pain, pain after eating fatty foods, fever or chills, nausea and vomiting, jaundice light-brown pee or light-coloured poo.
Conditions affecting the gallbladder
Several conditions can cause problems in your gallbladder, including:
gallstones (cholelithiasis), commonly caused by high cholesterol
gallbladder inflammation (cholecystitis)
gallstone pancreatitis (inflammation of the pancreas caused by a gallstone blocking the common bile duct and pancreatic duct)
gallbladder polyps (non-cancerous growths)
gallbladder cancer
Diagnosing gallbladder diseases
abdominal ultrasound is the most frequently used diagnostic imaging scan used to detect gallstones and cholecystitis
imaging scans including endoscopic ultrasound, CT scan and X-ray may be used to detect duct stones and gallbladder cancer
MRCP (magnetic resonance cholangiopancreatography) may be used to provide detailed imaging of the bile ducts and biliary system where other imaging tests have been inconclusive
Bile duct disease
Your bile ducts connect the organs in your biliary system. They are responsible for carrying the bile created by your liver and stored in your gallbladder to your small intestine.
If your bile ducts are affected by disease, bile can become blocked (obstructed) and back up into the other organs in your biliary system. This can cause inflammation and damage to those organs, which can result in cholecystitis (gallbladder inflammation), gallstone pancreatitis, liver cirrhosis, infections and cancer. Blocked bile ducts can also impact digestion, which can lead to malabsorption and malnutrition.
Common bile duct diseases
Common conditions affecting the bile ducts include:
bile duct stones (choledocholithiasis)
bile duct inflammation (cholangitis)
primary sclerosing cholangitis (PSC) (a chronic liver disease)
bile duct cancer (cholangiocarcinoma)
Diagnosing bile duct diseases
EUS (endoscopic ultrasound)
MRCP (magnetic resonance cholangiopancreatography) can be used to assess the bile ducts and identify blockages
blood tests may be done to measure liver function, which can indicate bile obstruction
Why choose Welbeck?
At Welbeck, our gastroenterology specialists are experts in hepatobiliary disease and are experienced in caring for and treating patients with conditions affecting the liver, gallbladder and bile ducts.
With access to colleagues across other specialities, our consultants are also able to refer within the Welbeck ecosystem if needed to ensure you receive the best possible treatment as quickly as possible, all under one roof.
All appointments, testing, treatment, and follow-up appointments take place within our state-of-the-art facilities, enabling us to deliver accurate diagnostics and advanced treatments.
Book your private consultation
Your health is important to us, so we strive to offer same-day appointments whenever possible.
Our consultants are recognised by the major health insurance companies. If you have private health insurance, your treatment at Welbeck can begin once you have obtained authorisation. We also provide care to self-paying patients. Learn more about the different payment options at Welbeck.
FAQs
What are the warning signs of hepatobiliary disease?
Hepatobiliary disease can cause a wide range of symptoms, including:
jaundice
abdominal pain
fever or chills
nausea or vomiting
loss of appetite, which may lead to weight loss
fatigue
itchy skin
light-brown pee or light-coloured poo
Can hepatobiliary disease be prevented?
Some hepatobiliary disease conditions, like liver disease, can be prevented through lifestyle changes such as eating a balanced diet, avoiding alcohol, exercising regularly and getting vaccinations.
What foods should I avoid if I have hepatobiliary disease?
If you have hepatobiliary disease, your consultant may advise you to avoid foods that are high in sugar, salt and saturated fat, and to stop drinking alcohol.
How serious is hepatobiliary disease?
The severity of hepatobiliary disease can range from relatively minor to very serious. Early detection and treatment are key to preventing complications and limiting disease progression.
