Can a HyCoSy improve fertility?
HyCoSy is an investigation to look at tubal patency (to check if the tubes are open) and there are some studies that suggest after HyCoSy the chances of natural conception/pregnancy is slightly higher.
What is the difference between a Hysterosalpingogram (HSG) and a HyCoSy test?
The procedure is exactly the same, but HyCoSy looks at the tubes and the womb with ultrasound, whilst HSG uses low dose X-ray. Depending on what your doctor is looking for, one test may be more suitable than the other.
What happens during a HyCoSy procedure?
You will be asked to change into a hospital gown. A sample pot will be given to you for a urine sample as we may do a pregnancy test (please come with a full bladder).
Your consultant will take a brief history from you and consent you for the procedure.
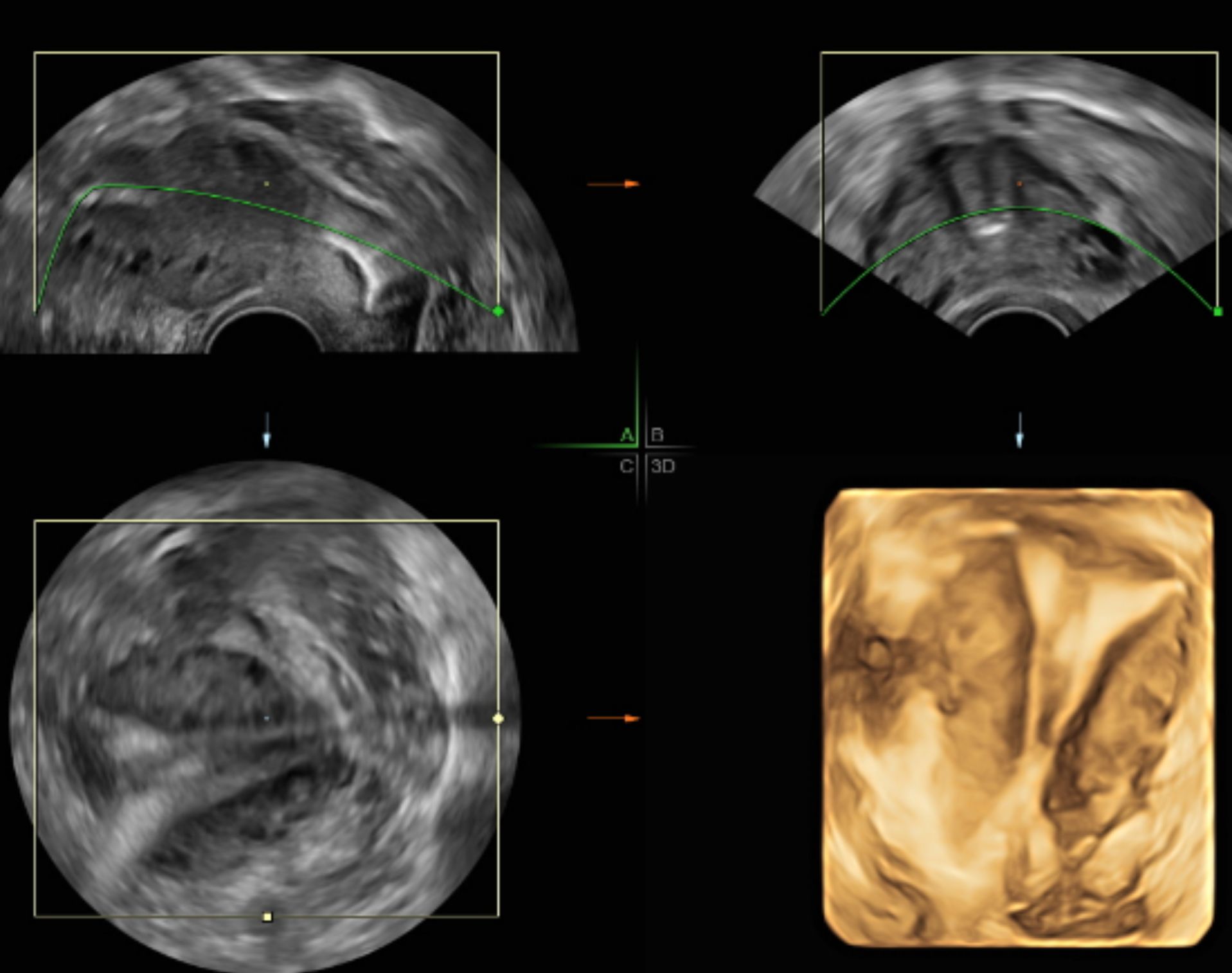
An internal (transvaginal) ultrasound will be performed first to ensure normal findings in the uterus (womb), ovaries and no signs of pelvic collections or infections.
You will be asked to lie on the examination table and the consultant will insert an instrument called a speculum into the vagina to hold the walls apart so that the cervix can be seen (the same procedure as having a smear test performed). A small thin, soft tube will be inserted into the cervix and liquid (saline or foam) will then be injected slowly into your uterus.
The speculum is then removed, and the transvaginal probe is again inserted. The flow of the contrast is monitored with the ultrasound until the liquid is seen passing along the fallopian tubes and eventually (if there are no blockages) spilling out at the ends into the pelvis. You may experience some discomfort with mild ‘period-like’ cramps as the fluid is injected. This should not be severe and generally settles quickly. Overall, the procedure takes about 25-35 minutes.
For more information about the procedure at OneWelbeck, please read our HyCoSy patient booklet.
What does the HyCoSy procedure at OneWelbeck include?
The procedure includes a consultation with a consultant, and a detailed transvaginal ultrasound scan and Antral follicle count which is all inclusive in the price package.
Unlike other centre's, the HyCoSy procedure at OneWelbeck uses saline followed by foam to assess the cavity and check tubal patency which is all included in the price. This is then followed by a detailed explanation of the results.
This procedure can be self-referred and can be booked directly via the website.
When do I receive the results?
Provisional findings are provided by your consultant directly after the procedure within the same consultation.
What determines the success of HyCoSy? – What if my test is abnormal?
Upon completion of the HyCoSy, your results will be given to you. If the results are abnormal – e.g., if the tubes are blocked, the doctor will explain the next steps which may include another procedure to open the tube, or further gynaecological assessment such as an MRI. Not all abnormal results require further intervention, but this will be explained to you at your consultation.
Is HyCoSy painful?
Most people find HyCoSy uncomfortable but not painful. During the procedure, the consultant will check how much discomfort you are in and adjust their technique accordingly. Most people experience “period-like” cramps when the fluid is injected.
What are the potential side effects or risks of HyCoSy?
With the HyCoSy there is a 1% risk of infection – this risk is reduced with a single dose of antibiotics given to you immediately after the procedure. And in some cases, the procedure may not be completed for example, your cervix may not be visible or the fluid leaks out. In such cases, we will rearrange the procedure for you, free of charge.
Can I have sexual intercourse after HyCoSy treatment?
Yes! We encourage this. As HyCoSy is a form of flushing of the tubes, there is a theory that natural conception may be higher after this procedure. Therefore, we encourage the patient to attend conception. You can have intercourse from that evening. Please note that there is no guarantee that HyCoSy will result in conception.
When is the best time to book a HyCoSy procedure?
It is best to book the test at least 24 hours after menstrual bleeding stops and before ovulation.
The HyCoSy can be done anytime from when you stop bleeding, up to day 18, however we recommend the test to be done prior to your ovulation cycle which is usually between days 5 to 14 (this can vary from person to person). If you are having a HyCoSy after an operation, you must have a normal period before you can have the procedure.