There are various avenues to take when it comes to managing APLS.
Risk factor reduction - the ones we know - blood pressure, weight, cholesterol etc. If you're diagnosed with APS, it's important to take all possible steps to reduce your risk of developing blood clots.
Effective ways of achieving this include:
- quit smoking
- eating a healthy, balanced diet – low in fat and sugar and containing plenty of fruit and vegetables
- taking regular exercise
- maintaining a healthy weight and losing weight if you're obese (have a body mass index of 30 or more)
Primary prevention - what happens if the antibody test is positive?
- Aspirin- no strong support for this at 75mg or 300mg.
- One study suggest a 1.8% annual event rate, another 5.3% when all there antibodies are positive. Aspirin did not help.
Secondary prevention - what should you do if you have had a clinical event?
- Warfarin with INR 2-3 vs INR 3-4? The evidence base is weak- bleeding risk goes up with INR 3-4, without definite benefit- it tends to be used when there is arterial clot.
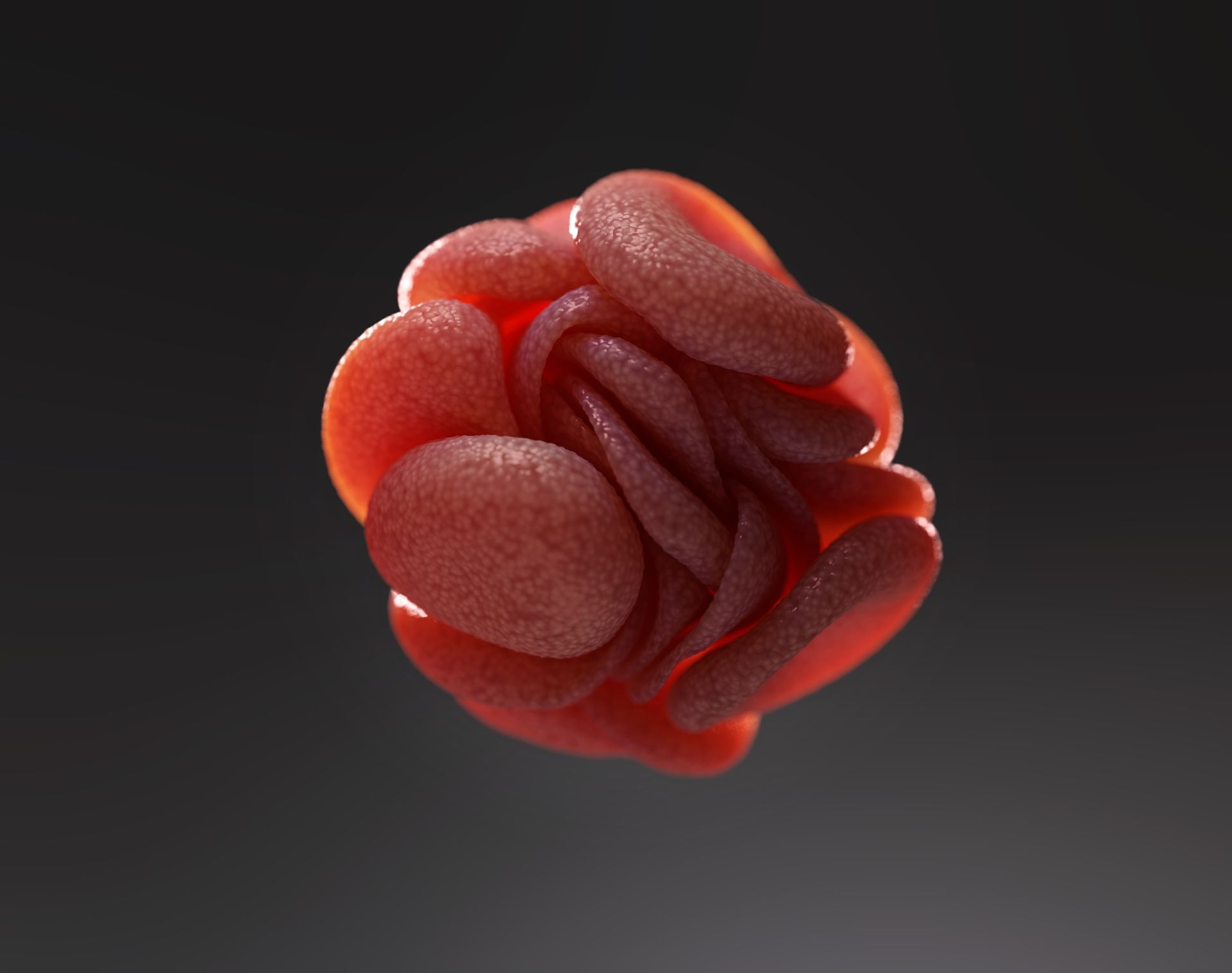
- Catastrophic APLS- this thankfully rare issue is treated with anticoagulation (warfarin or heparin), steroids, and plasmapheresis (washing the blood to get rid of the antibodies).
Pregnancy issues
- There is a recommendation of 75mg-150mg after 12 weeks gestation, and definitely by 16-20 weeks to reduce pre-eclampsia. The evidence is weak.
- Recurrent miscarriage in the past with APLS. The evidence is weak, but aspirin 75-150mg and low dose heparin tends to be given, in hope rather than conviction.
- Patients with APLS without a history of clots getting to second and third terms of pregnancy are often given aspirin subcutaneous heparin.
Patent Foramen Ovale (PFO) - what should you do if you have both APLS and PFO?
- 25% of the population have a PFO - if you have never had a clot, it is NOT a risk factor for clot and does NOT need to be closed.
- If you have had a clot, consensus in the USA guidelines, which I agree with, is that a large shunt across your PFO means risk of clot travelling from veins to arteries and the PFO should probably be closed.