Osteoarthritis, sometimes called degenerative joint disease (DJD), is the most common type of arthritis, affecting around 8 million people in the UK. The condition typically affects people over the age of 50, but it can affect younger people too, especially if a joint has suffered an injury.
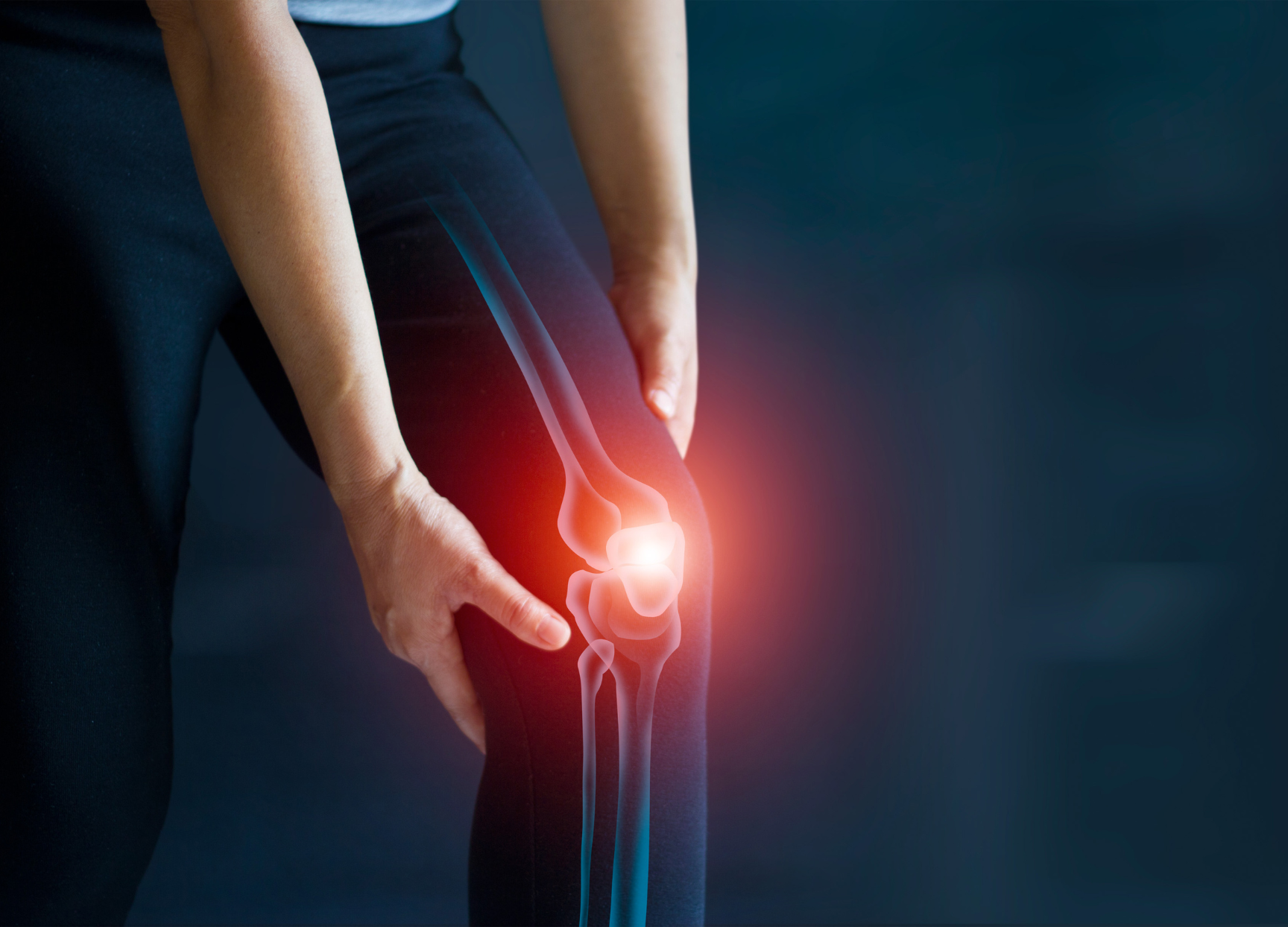
The condition causes the joints to become painful and stiff due to wear and tear of the surrounding cartilage and changes in the underlying bone. Although it can affect any joint in your body, osteoarthritis is most likely to affect weight-bearing joints or very active joints such as those in your hands, knees, hips, lower back and neck.
Meet one of our experts