Motor Neurone Disease
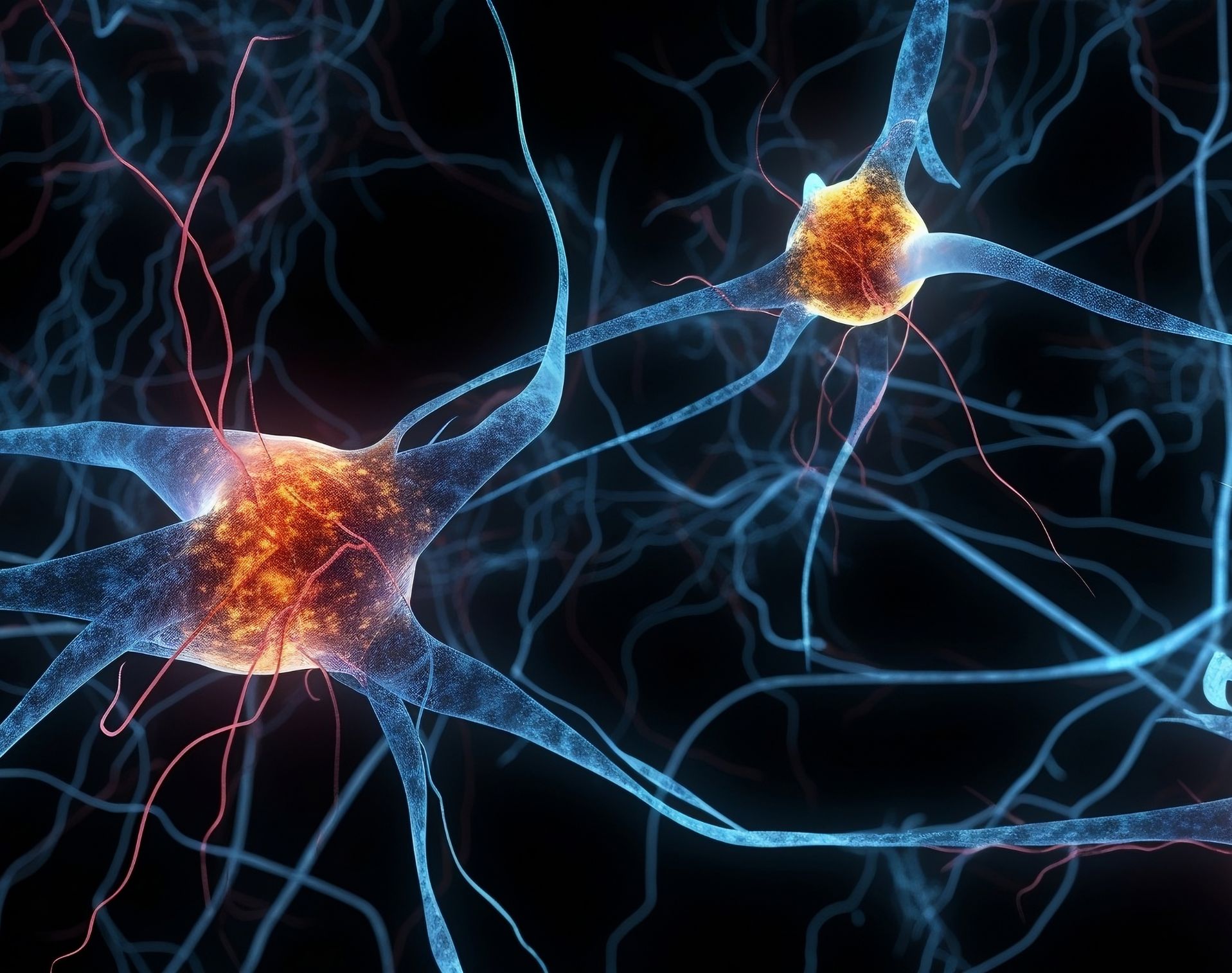
Motor Neurone Disease (MND) is a progressive neurological disorder that affects the motor neurons in the brain and spinal cord.
What is motor neurone disease?
Motor neurone disease (MND), also known as amyotrophic lateral sclerosis (ALS) or Lou Gehrig's disease, is a progressive neurological disorder that affects the motor nerves in the brain and spinal cord. Motor neurons are nerve cells responsible for transmitting signals from the brain to the muscles, enabling voluntary muscle movement and control.
In individuals with motor neurone disease, these motor nerves gradually degenerate and die, leading to a progressive loss of muscle function and movement.
At Welbeck, our leading neurologists diagnose and treat patients with MND in our dedicated Neurology centre.
What are the symptoms of motor neurone disease?
Motor Neurone Disease presents with a range of symptoms that primarily involve the motor neurons. Symptoms vary from person to person, and the progression of the disease can also differ. These are some of the more common symptoms:
muscle weakness: progressive weakness in the limbs is one of the earliest and most common symptoms. It may start with slight difficulty in performing everyday tasks that require fine motor skills, like buttoning a shirt or holding a cup
muscle wasting (atrophy): the affected muscles may start to waste away due to lack of use and degeneration of motor neurons. This can result in noticeable shrinking of your muscles
muscle cramps and twitches: some people with motor neurone disease may experience muscle cramps, spasms, or fasciculations (involuntary muscle twitches)
difficulty with speech and swallowing: as the disease progresses, muscles controlling speech and swallowing become affected, leading to slurred speech and difficulty in swallowing food and liquids
muscle stiffness and spasticity: in some cases, individuals with MND may experience stiff muscles and involuntary muscle contractions, which can contribute to difficulty in movement
tripping and falling: weakness in the legs can lead to balance problems, increasing the risk of tripping and falling
respiratory issues: as the disease progresses, the muscles responsible for breathing can be affected, leading to shortness of breath and respiratory difficulties
fatigue: individuals with MND may experience fatigue and find that their muscles tire easily with even minor exertion
It's important to note that motor neurone disease is a progressive condition, meaning that symptoms get worse over time as more motor nerves are affected and lost. The rate of progression can vary significantly among individuals – in some cases, the disease may progress rapidly, while in others, it may progress more slowly.
What causes motor neurone disease?
The exact cause of MND is not fully understood, and it’s likely to result from a combination of genetic and environmental factors. Some key factors believed to play a role in the development of the condition include:
genetic factors: in some cases, motor neurone disease is believed to have a genetic component. Several genes have been associated with the inherited form of MND, which accounts for around 5% to 10% of all cases. Mutations in these genes can lead to abnormal functioning of motor neurons, resulting in their degeneration and death. One of the most well-known genes associated with familial MND is the C9orf72 gene. Other genes linked to MND include SOD1, TARDBP, and FUS, among others
environmental factors: some research suggests that exposure to certain toxins or chemicals, such as lead, pesticides, or heavy metals, may increase the risk of developing MND. However, the association between these factors and the disease is still being investigated
glutamate excitotoxicity: glutamate is a neurotransmitter involved in nerve cell communication. In MND, there’s evidence of excessive levels of glutamate accumulating in the spaces between neurons, leading to a phenomenon called excitotoxicity. This excess glutamate can cause damage to motor neurons, leading to their degeneration
oxidative stress: oxidative stress occurs when there’s an imbalance between free radicals (reactive oxygen species) and the body's ability to neutralise them with antioxidants. Oxidative stress can cause cellular damage, including damage to motor neurons, contributing to the progression of MND
neuroinflammation: inflammation in the nervous system, known as neuroinflammation, has been found to play a role in the development and progression of MND. Immune system cells and inflammatory molecules may damage motor neurons, accelerating the disease process
Motor neuron disease is a complex and multifactorial disorder, and the effects of genetic susceptibility and environmental influences likely vary from person to person. In most cases, the specific cause of MND remains unknown, and it may be a combination of various factors.
How is motor neurone disease diagnosed?
Since the symptoms of motor neuron disease can resemble those of other neurological disorders, a comprehensive medical evaluation, including neurological examination and various tests, is essential to reach a diagnosis. Early diagnosis allows for better management of symptoms and access to appropriate care and support.
Tests to make and confirm a diagnosis of MND, and to rule out other conditions, may include:
- nerve conduction studies and electromyography (EMG)
- an MRI scan
- blood tests
- spinal tap (lumbar puncture)
- genetic tests
Can motor neurone disease be prevented?
Unfortunately, there’s currently no known way to prevent motor neuron disease.
What are the complications of motor neurone disease?
Motor neuron disease is a progressive disease – over time, you may experience more symptoms, and the severity of your symptoms will worsen.
Treatment can help you manage these symptoms, but unfortunately, MND cannot be cured and is life-shortening.
What are the treatment options for motor neurone disease?
Unfortunately, there’s currently no cure for motor neuron disease. However, there are various treatment options and supportive measures available to manage the symptoms, improve quality of life, and keep you comfortable. Riluzole, the only licensed treatment for MND, has been shown to lead to a moderate improvement in survival. Management of late breathing muscle weakness with non-invasive ventilation has also been shown to lead to an improvement in quality of life.
The management of MND often involves a multidisciplinary approach. At Welbeck, our experienced neurologists develop tailored treatment plans that address the unique features of your condition and meet your specific needs. They work closely with consultants in other specialities to make sure you receive the care you need, across all areas of your health and wellbeing.
Some of the key treatment options and supportive measures for MND include:
medications: there are certain medications that may be prescribed to manage specific symptoms of MND. There are certain medications that may help slow the progression of the disease and extend survival in some cases. Other medications may be used to address symptoms like muscle cramps, pain, spasticity, and excess saliva
physical therapy: physical therapy plays a crucial role in managing MND. It can help you maintain mobility, prevent joint stiffness, and improve muscle strength. Physical therapists can recommend exercises and assistive devices tailored to your individual needs
occupational therapy: occupational therapy focuses on helping individuals maintain their independence and functionality in daily activities. Occupational therapists can suggest adaptive techniques and devices to assist with self-care, communication, and mobility
speech therapy: as MND can affect speech and swallowing, speech therapists can help improve your communication skills and teach you strategies to cope with speech difficulties. They can also provide guidance on safe swallowing techniques
respiratory support: as the disease progresses and affects the muscles responsible for breathing, respiratory support may be necessary. This can include non-invasive ventilation (NIV) or, in some cases, invasive ventilation (tracheostomy ventilation) to assist you with breathing
nutritional support: as swallowing difficulties can lead to malnutrition and weight loss, a dietitian can provide you with advice on proper nutrition and recommend ways to ensure you are getting enough calories
assistive devices: various assistive devices, such as wheelchairs, communication devices, and computer adaptations, can significantly improve your quality of life and independence
emotional and psychological support: MND can be emotionally challenging for you and the people close to you. Access to counselling, support groups, and mental health services can provide emotional support and coping strategies
hospice and palliative care: in advanced stages of MND, hospice and palliative care services can provide comfort and symptom management to improve the patient's quality of life
At Welbeck, we work closely with our patients, providing regular monitoring and adjustment to treatment plans to meet your needs as your disease progresses. Clinical trials and ongoing research are also exploring new therapies and potential treatments for MND, providing hope for future advancements in managing the disease.
Why choose Welbeck?
At Welbeck, our neurologists are experts in their field and are dedicated to providing world-class care to every patient.
With access to colleagues across other specialties, our consultants are also able to refer within the Welbeck ecosystem when required to ensure you receive the treatment you need as quickly as possible, all under one roof.
All appointments, testing, treatment, and follow-up appointments take place within our state-of-the-art facilities, enabling us to deliver accurate diagnostics and advanced treatments.
Book your private consultation
Your health is important to us, so we strive to offer same-day appointments whenever possible.
Our consultants are recognised by the major health insurance companies. If you have private health insurance, your treatment at Welbeck can begin once you have obtained authorisation. We also provide care to self-paying patients. Learn more about the different payment options at Welbeck.
Get in touch today to book an appointment.
FAQs
Can genetic testing tell me if I’m at risk of MND?
Yes. While only 5% to 10% of MND cases are linked to genetics, testing can be done to help evaluate your risk and explore options such as counselling or participation in clinical trials.
Will I still be fully aware, emotionally and mentally, as the disease progresses?
For most people with MND, cognitive functions and mental awareness remain intact. However, about half may experience changes in behaviour or thinking, and a smaller number may develop frontotemporal dementia, where memory or emotional control is affected.
How common is motor neurone disease?
MND is considered a rare condition. In the UK, it affects roughly 2 in every 100,000 people each year, with most diagnoses made between the ages of 50 and 70.
Does motor neurone disease affect life expectancy the same way for everyone?
MND progresses differently from person to person. Some people experience faster changes, while others live with the condition for many years. The type of MND you have, your age at diagnosis, and your overall health all influence how the condition develops.
What is motor neurone disease?
What are the symptoms of motor neurone disease?
What causes motor neurone disease?
How is motor neurone disease diagnosed?
Can motor neurone disease be prevented?
What are the complications of motor neurone disease?
What are the treatment options for motor neurone disease?
Why choose Welbeck?
Book your private consultation
FAQs
