
Professor Michael Polkey
Specialist expertise: COPD, Sleep, Snoring, Home Ventilation, General Respiratory Medicine, Respiratory Medicine.
Breathlessness is a symptom we commonly see patients suffering from at OneWelbeck Lung Health. Professor Michael Polkey, Consultant Respiratory Physician at OneWelbeck and Royal Brompton Hospital, explains the various causes behind this symptom.

Oxygen is required for all organs of the body. The main function of the lung is to get oxygen (the ‘good gas’) into the body and to get carbon dioxide (the ‘bad gas’) out. To do this air is pumped in and out of the lungs by the breathing muscles but how hard they must pump depends on what the person is doing and whether any disease of heart or lungs is present. For instance, when somebody goes for a run the ‘pump’ needs to work harder in order to supply enough oxygen to the exercising muscles. However, because the person knows that they have gone for a run they expect to need to breathe harder and so they don’t normally regard this as abnormal (even though they might be ‘puffed out’ after the run).
An individual experiences breathlessness when they feel an increased need to breathe when they don’t expect to need to. Why might this occur? To understand this, we need to understand how oxygen enters the body and reaches its target. Although there are some technical differences the carbon dioxide essentially makes the reverse journey.
The oxygen starts in the air outside the patient and must travel through the airways to the most distal lung unit, the alveolus. The alveolus is separated from the blood by a single cell which the gases can migrate across. The oxygen is then carried by the blood to the organs that need it. Breathlessness can occur if any stage of this pathway is interrupted since if so, the patient's breathing pump would need to work harder to deliver the oxygen to the end organs and this is experienced as breathlessness.
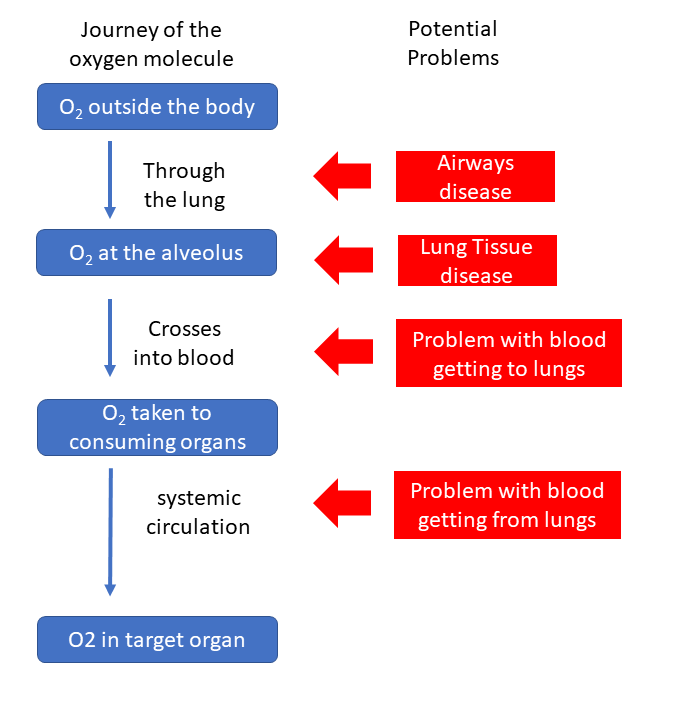
In a sense any unexpected breathlessness is worrying and should prompt medical review. However, doctors tend to be most worried about severe breathlessness which comes on quickly or suddenly; the reason why doctors worry about this is because if it progresses the patient may eventually be unable to get enough oxygen into their lungs or even die. In that situation urgent review is necessary most usually at their local accident and emergency department. Common examples of underlying causes of this might include acute severe asthma (an airways problem), COVID-19 (a problem of the lung tissue which becomes non-functional due to viral inflammation) or pulmonary emboli (where blood clots in the blood vessels stop blood going to the lung).
The following is a brief guide but of course a great many conditions, some very rare, may also cause breathlessness.
In the airways the most common condition in adults is Chronic Obstructive Pulmonary Disease in which lung mechanics worsen, most commonly as a result of previous tobacco consumption. Other features may include cough or daily sputum production.
In the lung tissue the most common condition would be a family of diseases (termed interstitial lung diseases) in which the alveolus becomes non-functional due to non-infectious causes, often inflammatory but sometimes occupational (for example asbestosis). Again, this may be associated with cough though this is usually dry and non-productive
In the pulmonary circulation the blood supply to the lung may be chronically reduced as a result of blood clots on the lung, but resistance in the pulmonary artery may also increase spontaneously (Primary pulmonary hypertension). If there is anaemia the heart will need to pump the blood more rapidly to achieve the same oxygen transport.
Finally, if there is a problem with the pumping action of the heart the blood may not be pumped efficiently away from the lungs. This can occur if there is a problem with the heart muscle itself and if there are problems with the valves within the heart.
Clearly your doctor will wish to hear your story in more detail and may ask specific questions if the story suggests it. S/he will wish to examine you to look for physical signs but investigations which will almost certainly be considered necessary are:
Depending on what these tests show other subsequent possible tests necessary are:
What causes breathlessness normally?
What causes symptomatic breathlessness?
The normal path of an oxygen molecule
What are the common causes of this pathway interruption and when should I be worried?
What are common causes of slowly progressive breathlessness?
Which tests might help sort this out?
Here at OneWelbeck, we have a team of exemplary respiratory specialists, state of the art facilities and diagnostics, and highly competitive financial packages for self-funding patients as well as those with private health care.
Lung HealthProfessor Michael Polkey is Professor of Respiratory Medicine at Imperial College and has published almost 300 peer reviewed scientific articles. Professor Polkey was elected a Foundation Fellow of the European Respiratory Society in 2014 and awarded the Gold medal of the ERS for his research in COPD in 2018.